BPSU quotes and recommendations
“We want to find out how common this condition is across the UK and Ireland”
“We also hope that this surveillance will raise awareness of the condition amongst paediatricians”
“The BPSU will provide useful information about the condition for doctors looking after children with such conditions, public health specialists and researchers who would like to better understand the condition and develop effective treatments.”
“It is likely that these (cases that did not meet the case definition) were milder cases along the PIMS-TS spectrum, which needs to be taken into account in future case definitions”
“Mild cases and those that were not hospitalised or had short hospital stays, may therefore be missed”
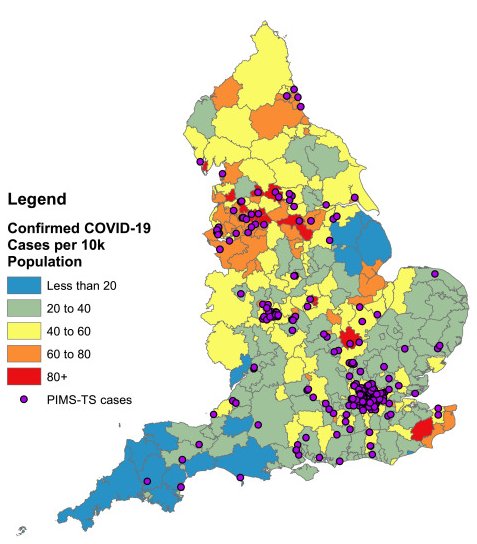
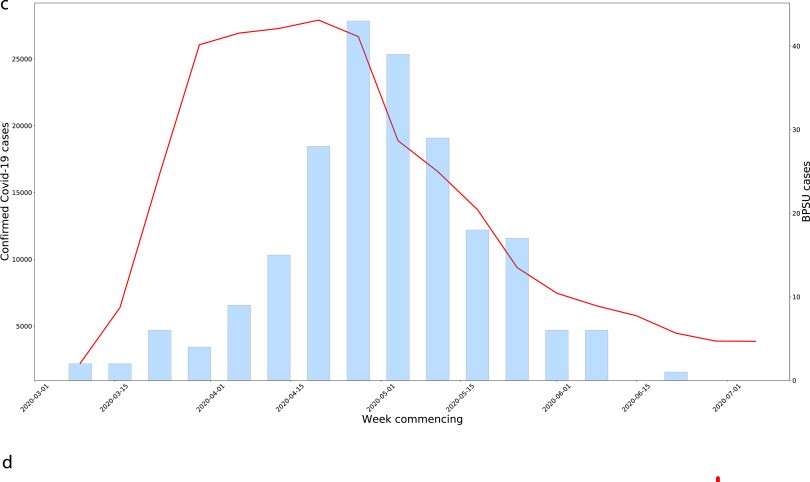
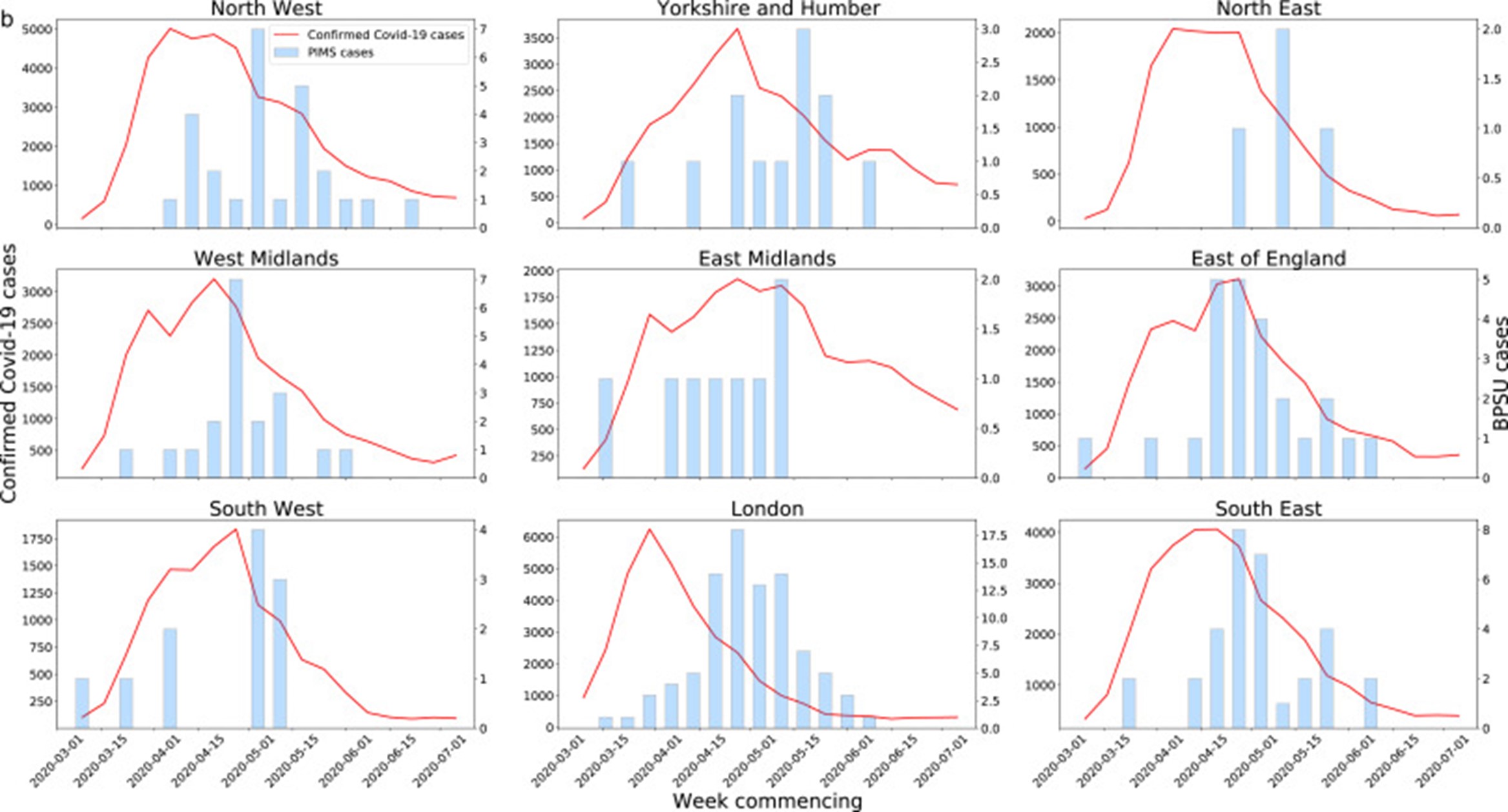
“The strong association between SARS-CoV-2 and PIMS-TS emphasises the importance of maintaining low community infection rates to reduce the risk of PIMS-TS. Understanding the relationship between SARS-CoV-2 and PIMS-TS could provide useful insight into the pathogenesis of both KD and TSS. Close follow up will be important to monitor rapidly changing epidemiology as well as the short to long term complications in children with PIMS-TS.
(Source BPSU Study)
Our questions arising from the study
- You mention the possibility of cases of incomplete or atypical PIMS-TS and the need for the definition of PIMS-TS to be widened. How will this be disseminated and acted upon following your study findings?
- What is being done to ensure the follow up of known PIMS-TS cases that you recommend in your study?
- You mention the challenges of collecting data on PIMS-TS, KD and TSS. What action needs to be taken and by who to remedy this?
- You mention the importance of minimising transmission of COVID-19 in children to reduce cases of PIMS-TS. What action needs to be taken and by who to achieve this this?
- Has incidence of PCR and antibody testing been improved, as a result of the study?
- When will a much- needed active surveillance system be set up for PIMS-TS, KD and TSS, so that the public can have access to up to date real time data so that researchers can easily access data to further investigate the links between these 3 conditions and potentially Long COVID too?